 President's Message
President's Message
Mary Moore

As I write this on May 3, I have to say that March and April have been very different from any other two months that I can remember. We have seen our country and the world brought to their knees by a microscopic virus. It has been inspiring to see so many people pull together and help each other. I have become a huge fan of Gov. Cuomo in New York, and have deep appreciation for the sacrifices and courage shown by so many doctors, nurses, first responders, bus drivers, grocery workers, and so many more. Then there are the parents who are working from home and also helping their children attend school remotely. And there are the clinical social workers and other mental health providers who help support everyone who is lucky enough to get their help. You, our members, are front line workers in hospitals or are support for front line workers, or support for everyone else who is coping with this pandemic. I salute you and thank you for your service. The mental health toll that this is taking is high and the continued toll has not even been felt yet, but is widely anticipated.
I don’t think there has been anything like this that affects everyone in our country since World War II. There have been epidemics (HIV/AIDS); attacks (9/11) and economic collapses (the Great Recession). This current crisis seems to have it all rolled into one and no one is exempt. Everyone has a part to play. I have been inspired that so many took it seriously in March to “shelter in place”, many of whom at that time didn’t realize how much it can affect all ages, and sacrificed their freedom and livelihoods for the sake of their parents and grandparents.
It will be interesting to see how our practices and the Society continue to evolve as we move forward in a country still very much infected with the virus. I encourage you all to keep up with self-care, spend time talking with friends, colleagues, your own therapist and family. As we hold space for our clients, we need someone to hold space for us, as we are coping with it, too. Even harder, some of us have lost family and friends to the virus. My heart goes out to you.
Your membership dollars, directed by the Board, made a contribution to local food banks ($5,000), the Clinical Social Work Association ($3,000) and the Pro Bono Counseling Project ($2,000). We plan to reassess in June and make another contribution .
The Society has been a big help to many of us via the Listserv, when we had to convert our practices to video sessions. Lots of figuring out and sharing about health insurance coding and various platforms. Thank you very much to Judy Gallant, Margot Aronson, Laura Groshong and Melissa Grady for compiling the “Toolkit for Virtual Practice”, which is posted on the GWSCSW.org website. It has been a big help.
We had to cancel our Annual Membership Dinner and Volunteer Brunch, and have begun converting continuing education events to webinars. In thanks to our volunteers, we sent individual gifts to each of them (live plants). Thank you to Beverly Magida, Nancy Harris, Irene Walton, Catherine Lowry and Philip Callahan for the work they had already put into the Annual Dinner and the work of canceling it. And thank you, Beth Pascoe, for coordinating the Volunteer Brunch, canceling it, and then, with Suzanne Cooper, sending the gifts to our 47 dedicated volunteers. We also shifted more energy into “Coffee Houses,“ "Happy Hours,” “Early Career Get-Together” and other virtual opportunities to connect with each other.
This is my last “Letter from the President,” as my two-year term comes to a close on June 30. I have enjoyed serving as your President and will continue to assist with Society leadership. I am to be followed by Lynn Grodzki, a member with a rich resume which includes authoring six books, presenting at national conferences, past vice president of NASW-Metro Chapter 2011-13. Lynn is also a member of the Cosmos Club, nominated as a distinguished social worker.
Thank you all for being there for the rest of us. You are very special people. Stay calm and carry on.
GWSCSW sends Congratulations to our Incoming Officers and Branch Directors!!
|
President: Lynn Grodzki |
Director of Communications: Steve Szopa |
Let us all give them a big welcome and lots of support as they take the helm on July 1, 2020!!
 GWSCSW TOOLKIT FOR VIRTUAL PRACTICE DURING THE COVID-19 NATIONAL EMERGENCY | APRIL, 2020
GWSCSW TOOLKIT FOR VIRTUAL PRACTICE DURING THE COVID-19 NATIONAL EMERGENCY | APRIL, 2020
Judy Gallant, LCSW-C, Director, GWSCSW Legislation & Advocacy Branch
This toolkit can be found on the GWSCSW Website at: COVID Toolkit
Please note: This information is not to be construed as legal advice. It is being posted with links to additional information, and further research may be required. [ It is current as of 4/14/20.] * UPDATED ON 4/30/20.* Changes to the law as a result of the Covid-19 crisis can happen at any time, as Executive Orders issued by the Federal or State governments have been frequent since the national State of Emergency has been declared. If you are aware of any new/different information, please contact judy.gallant@verizon.net. We will do our best to keep this information updated, but cannot guarantee it is up-to-date at any given time.
We work closely with The Clinical Social Work Association, with frequent exchanges of practice-relevant information during this National Crisis. CSWA is also maintaining a helpful Toolkit (available to all) on their website.
CURRENT LAWS AND REGULATIONS
- Medicare will reimburse for telemental health therapy: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet The most recent information is that you can bill for telehealth from 3/1/20 until the end of the National State of Emergency.
- Updated information: LCSWs can now be reimbursed by Medicare for audio only psychotherapy sessions which have taken place as of 3/1/20 on. More details can be found at https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
For more detailed Medicare information, see pages 4-5 of this document.
- ALL LOCAL JURISDICTIONS (MD, VA & DC) ARE INDICATING THAT IT IS OK FOR TELETHERAPY TO OCCUR ACROSS STATE LINES FOR CONTINUITY OF CARE WITH CURRENT CLIENTS DURING THE DECLARED STATE OF EMERGENCY DUE TO THE COVID-19 VIRUS. In Maryland, there is an explicit order from our governor, with our licensing board interpreting how they are proceeding. In DC, explicit guidance has also been developed: if you are practicing from another jurisdiction in DC, there is no problem with providing continuity of care with clients with whom you have a prior relationship; establishing a new relationship gets complicated. In Virginia, the regulatory requirements have now been waived.
For MD, go to https://governor.maryland.gov/wp-content/uploads/2020/03/Executive-Order-Health-Care-Matters.pdf
The Board of Social Work Examiners (website: https://health.maryland.gov/bswe/Pages/default.aspx) is asking clinicians to submit an application in order to provide ongoing therapy through teletherapy, to already established client(s). It is free to apply, and it is reportedly not too onerous. Contact person to obtain an application: gloria.hammel@maryland.gov
- For DC: Waiver of Licensure Requirements for Healthcare Providers 20-03-13, and Guidance On Use of Telehealth in the District of Columbia 3-12-2020. We have just heard from a member that after writing to the DC Board to ask about establishing relationships via videoconferencing with new clients, she was given permission to do so prior to her DC license being processed. We would recommend that you check directly with the DC Board if you would like to do this.
· For VA: See https://www.dhp.virginia.gov/social/covid19Info.htm
Board of Social Work
COVID-19 Information
Accelerated Temporary License
April 20, 2020
Pursuant to Governor Northam’s Executive Order No. 57 (effective April 17, 2020), a clinical social worker with an active license issued by another state may be issued an accelerated temporary license by endorsement as a health care practitioner of the same type for which such license is issued in another state upon submission of an application and information requested by the applicable licensing board and the board's verification that the applicant's license issued by another state is active in good standing and there are no current reports in the United States Department of Health and Human Services National Practitioner Data Bank. Such temporary license shall expire ninety (90) days after the state of emergency ends. During such time the practitioner must seek a full Virginia license or transition patients to Virginia-licensed practitioners.
Health care practitioners with an active license issued by another state may provide continuity of care to their current patients who are Virginia residents through telehealth services. However, if they want to acquire new patients, they must apply for full licensure in Virginia or an Accelerated Temporary License as indicated above.
You can access the applications here: Temporary Licensed Clinical Social Worker Application
- For any state where your client is located during sessions, make sure that you check with the Board that governs social work practice in that state to see if you need to apply for a waiver, pay a fee, etc.
- At this writing, audio only telephone appointments are not reimbursable by insurance companies, except by Medicare. And an executive order signed by Gov Hogan approves reimbursement of telehealth sessions provided by telephone for health care providers who participate with Maryland Medicaid only…OR providers who are enrolled with MD Behavioral Health Administration programs. (This is also true for those participating in SAMHSA grant programs.).
PAYMENT, BILLING, CODING, CPT MODIFICATIONS
- Most commercial insurance plans will reimburse for telemental health therapy through video platforms, but the details depend on the specific plan. Patients should be asked to confirm with their insurance that reimbursement will be provided, and whether they are restricted to receiving it on a specific platform like Teladoc. BlueCross BlueShield and Aetna have lifted requirements that providers use Teladoc for telehealth sessions during the National Emergency, and will reimburse for sessions on HIPAA compliant platforms. See links below for coding modifiers to use for those insurances. Other insurances seem to be accepting a 95 modifier for the CPT code and 02 as the place of service. Medicare is asking 11 to be used at the place of service with the 95 modifier.
- Information from Aetna to cover sessions 3/6-6/4 2020: https://www.aetna.com/content/dam/aetna/pdfs/health-care-professionals/bh-televideo-service-codes-covid-19.pdf?cid=eml-prov17136150&spsub=prov_NTI0NjE5MDgyNjY4S0
- Information from BCBS re: coding for teletherapy: https://individual.carefirst.com/carefirst-resources/pdf/carefirst-telemedicine-code-modifier.pdf
- Additionally, CareFirst is amending its Medical Policy on a temporary basis to pay a $20.00 flat fee for phone consultations of 10-15 minutes provided by behavioral health providers in CareFirst’s network. “Psychiatrists and Nurse Practitioners should use CPT 99441. Psychologists, Licensed Certified Social Workers and Licensed Professional Counselors should use code 98966. We selected these codes, as check-ins for all phone visits, regardless of the amount of time. This is in effect through April 17, 2020. At the end of the 30 days
- CareFirst will re-evaluate whether the policy should be extended for a longer period.” As I understand this, the 98966 code can be used for a phone consultation - not a phone call to deal with scheduling issues, but a consultation where a clinical issue is addressed.
HIPAA PLATFORMS FOR TELEMENTAL HEALTH THERAPY
- HIPAA regulations are relaxed. As a result of the COVID-19 national emergency declaration, the Office of Civil Rights (OCR), Department of Health and Human Services (DHHS), has affirmed that it will “exercise its enforcement discretion and will not impose penalties for noncompliance with the regulatory requirements under the HIPAA Rules against covered health care providers in connection with the good faith provision of telehealth during the COVID-19 nationwide public health emergency.” See https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html.
- Although penalties are being waived, we should always strive to maintain client confidentiality to the best of our capacity. Currently, we are aware of three platforms - doxy.me, VSee, and Zoom - that each offer a Business Associates Agreement (BAA) to users as well as offering encryption to make the platforms more secure. Zoom’s platform offering those services is quite costly, but Zoom also offers free and less expensive platforms that do not have the same level of security. Doxy.me and VSee have free platforms that offer security, but which may not be systems that are as smooth to view as paying for additional speed within their platforms. There are likely others which are not included here.
- A major issue to note: although the OCR notification allows non-HIPAA-compliant platforms, it does not allow “public-facing” platforms. Facebook Live, Twitch, TikTok, and similar video communication applications are public-facing, and they should not be used in the provision of telehealth by covered health care providers.
CONSENT FORMS FOR TELEMENTAL HEALTH THERAPY
- If you are a member of the Clinical Social Work Association, you can download a sample Consent form for Telemental Health therapy at: https://www.clinicalsocialworkassociation.org/Informed-Consent-for-Telemental-Health
- We have found sample consent forms on other websites to be inadequate, lacking a place to record contact information for a local hospital or Crisis Center Hotline. Having a personal emergency contact is not enough, as you may be the person who needs to make contact for emergency services to be delivered during a teletherapy session.
ONLINE PAYMENT FOR PSYCHOTHERAPY
- Paypal and Venmo are not generally seen as secure even in privacy mode.
- Zelle is a bank-to-bank transfer, and requires the client’s bank to use this system, as well as your bank. You need only give your client a cell phone number or email address, no information about bank accounts is exchanged with your client.
- Ivy Pay is a system is exclusively for therapists’ use. There is a 2.75% fee. You charge the client’s debit, credit, HSA or FSA card on file. It is HIPAA compliant.
- Square is a secure platform that permits you to accept credit card payments. Fees are 2.75% per swipe or 3.75% plus 15 cents for manually entered transactions.
- A credit card can be kept on file and billed directly. Credit card fees vary.
- Bills may be sent via mail and clients may pay by check.
INFORMATION ON MEDICARE
- LCSWs can now be reimbursed by Medicare for audio only psychotherapy sessions which have taken place as of 3/1/20 on. More details can be found at https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
- CPT codes are the same as the ones that we use for in-person and videoconferencing sessions, e.g., 98034, 98037, 90791, etc. Any telephonic session that you have conducted since March 1 can be submitted for reimbursement.
- The POS code should continue to be 11 for Medicare claims. During the Public Health Emergency, the CPT telehealth modifier, modifier 95, should be applied to claim lines that describe services furnished via telehealth.
- This is the decision that CMS has made for Medicare coverage. As we know, private insurers often follow the lead of Medicare policy, so there is a chance that we will see more coverage of audio only sessions by private insurers. Do not take it for granted though, that this is the case. Continue to check the plan that each patient has if you wish to conduct treatment in an audio only format.
- This also will not automatically apply to ERISA, or self-insured, plans. We are continuing to pursue audio only coverage for those plans as well.
- New information and news releases can be found at https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
SOME CLINICAL ISSUES TO CONSIDER
Numerous clinical issues have emerged regarding the way we practice psychotherapy via telehealth. This list is by no means exhaustive, but it can be useful in thinking through ways to understand the impact these issues may have on our patients and ourselves and help us think about what we can anticipate and discuss with clients. We can reach out to our fellow therapists as part of our own support and taking care of ourselves. For our clients, it may all be worthy of exploration and is “grist for the mill.”
Seeing each other’s home environment
- In a virtual session, we are "seeing" clients in different places – we see them in their houses and they see you in yours. How do we feel about the loss of privacy we usually have with our clients? How do they feel about our having this visual window into their world? We and our clients can make some choices about what we want each other to see, with the option of exploring related therapeutic issues.
Boundaries
- What is the background view our clients see behind us on-line? What pictures or pets might they see, what noises might they hear, what is the potential for interruptions from family members? How might those things make your clients feel? How would you feel about them seeing those things?
- Try to protect the space you use at home from interruptions by posting a sign on the door – “In session. DO NOT ENTER” – and informing family beforehand that you will not be available during this time, and ask clients to do the same.
Feelings and concrete issues patients might have about receiving telemental health therapy
- Which of our clients might not want to receive psychotherapy in this format? Reasons could include feeling disconnected from the therapist with the computer screen between them, discomfort with the technology, lack of access to the technology, lack of private or safe space in their home, etc.
- We can appreciate that for some clients this platform feels comfortable and works well. Might this impact what format they want to continue receiving therapy with after the national emergency is over?
Feelings some therapists might have about providing videoconferencing
- Do we want to, or are we comfortable with using this format to provide psychotherapy? It can be important to notice: do we feel less engaged, or have more difficulty with “screen silence” than we would with silence in a room both you and your client are present in?
Distractions
- Are we, or our clients, distracted by things the other person cannot see, such as email, texts, etc? How easy is it for any of us to lose our focus in this environment?
Contribution of the electronic platform to our therapeutic work
- What nuances in the clinical encounter might we be missing, i.e.: the shift in affect that you feel when you are sitting with someone? The electronic platform, with delays and pauses, lack of synchronicity with visual and audio signals, presents general challenges of the medium.
- Does the medium impact client response; ie: might time delays impact your client’s reactions by them becoming more passive, for example?
- Does the screen permit some clients to express themselves more freely than in-person work does? What dynamics are at work that we can help the client look at to increase their understanding of the difference?
- What impact does the medium have on us? How does the screen impact our sense of engagement? Increased tiredness due to constantly having someone “in your face” hour after hour?
Technological problems
- When the technology for videoconferencing breaks down, patients may experience anxiety about the abrupt interruptions and this should be anticipated in discussion at the beginning of telemental health therapy. A plan for reconnecting with the patient should be agreed upon in advance, should the connection be lost.
Diagnostic criteria
- What risks might there be to seeing people with specific diagnoses via telemental health therapy? Some diagnostic criteria can make videoconferencing or telephone sessions problematic or potentially dangerous. We need to assess the level of suicidal or homicidal thoughts a client has and whether we can manage them successfully without being in the same room with them. Having clear boundaries in the informed consent about when the client may be referred to a different level of care is a prudent part of videoconferencing.
Uncertainty
- The questions around how long the pandemic and physical distancing will last creates anxiety for clients and therapists alike. In particular, we all feel uneasy about the length of time we will be unable to meet in person with our clients. Exploring this topic with patients, and understanding for ourselves how difficult we find this, can be helpful.
Support
- The GWSCSW list serve has provided both an exhaustive and exhausting series of announcements, updates, and helpful commentary from our members. Some members are offering webinars and/or discussion groups, some paid, some free. We are our own wonderful resource!
- CSWA is offering CE webinars on telemedicine, ethics, and more, free to members (and free for newly joining members), as well as “Get Together” sessions to provide support and connection.
- This is a time to reach out to one another, explore feelings, renew or develop new collegial friendships as we navigate this new world together….
ADDITIONAL RESOURCES
More helpful information from CSWA
Mental health resource
- This looks like a wonderful resource, which we learned of through CSWA’s collaboration with the Mental Health Liason Group. Scroll about a quarter of the way down the page and click on Mental Health Providers. https://psychhub.com/covid-19/
GWSCSW Annual dinner rescheduled to June 2021
Save early June (date to be announced) 2021 for GWSCSW Annual dinner. We had a lot of input from former attendees, the Board, and the general membership regarding making the 2020 dinner fun and special, with lots of interaction, networking and good food. Unfortunately, the pandemic is forcing us to put it off to 2021. But we won’t forget lessons learned and improvements planned. So we hope you join us then. Any questions please contact Beverly Magida (bev.magida@verizon.net) or Nancy Harris (nlharris1214@gmail.com).
Therapy in the Time of Covid-19
By Gina Sangster, MFA, MSW, LICSW | Psychotherapist & Supervisor, Capitol Hill Consortium for Counseling & Consultation
 During Week-1 of the shut-down, emails started piling up on the clinical social work list serve with countless questions about virtual platforms: who uses Doxy.me? Who likes Spruce? Which one is the most affordable? Will the various Boards that govern our practices allow us to be paid for working virtually? What about payment? Is Venmo secure? What about PayPal? Luckily, by the end of the week, most clinicians in the larger community were finding their way and of course being helpful to one another.
During Week-1 of the shut-down, emails started piling up on the clinical social work list serve with countless questions about virtual platforms: who uses Doxy.me? Who likes Spruce? Which one is the most affordable? Will the various Boards that govern our practices allow us to be paid for working virtually? What about payment? Is Venmo secure? What about PayPal? Luckily, by the end of the week, most clinicians in the larger community were finding their way and of course being helpful to one another.
The reality is, I’ve been completely dependent on our practice management and all the admin staff that clients typically see when they come to our offices for therapy. The speed and efficiency with which our practice transitioned to Zoom is nothing short of awe-inspiring. Of course some clinicians – as well as many clients – are more accustomed to virtual technology than others. It was a client who explained the “gallery format” to me that allows everyone in a Zoom group to see and hear everyone else! For someone like me, who remembers when correcting typewriters were cutting edge, becoming adept at using Zoom has been surprisingly gratifying.
But what about the actual content of the therapy sessions? How do we sense the mood in the room when the rooms are separated by miles and only visible on a screen? I’ve found this aspect of the experience to be the most rewarding – and surprising. When we first started discussing the plan to go virtual, a colleague of mine and I were probably among the most skeptical, both of us adhering to a more analytical, long-term, deep-dive approach to therapy than other more solution-focused models that may seem more adaptable to technology. For most clients – and therapists – it seems the inhibitions we feared would be a barrier, the awkwardness of distance versus face-to-face have melted away and the work of self-reflection, understanding, exploration and healing are continuing uninterrupted.
It’s true that for some, the shift from in-person therapy to virtual has been difficult, just as the edict to stay home has been more difficult for some than others. For people who naturally enjoy alone time or quiet time at home, or for those who typically work from home anyway, the current situation is easier to manage. For those who rely heavily on external sources of enjoyment and self-care, having the gym and restaurants all closed is more difficult. I believe all of us are struggling to find a way to connect with others while having to keep our “social distance.” I’m grateful that I can still do the work I love and “see” my clients, as well as some of their cats and dogs.
 POSTING TO THE GWSCSW LISTSERV - To post to this group, send email to: listserv-gwscsw@googlegroups.com
POSTING TO THE GWSCSW LISTSERV - To post to this group, send email to: listserv-gwscsw@googlegroups.com
If you are not on the listserv, contact admin@gwscsw.org
By Gina Sangster, MFA, MSW, LICSW | Psychotherapist & Supervisor, Capitol Hill Consortium for Counseling & Consultation
Most therapists work hard to maintain appropriate boundaries with clients. Many of us have heard stories of the “over-sharing” therapist who talks too much about his or her personal life, leaving the client feeling lost and unsure of how or if they can make good use of the time. In clinical meetings, we often discuss the valuable uses of self-disclosure and the importance of timing: not saying too much too soon but being able to interject a meaningful detail about one’s life experience when we assess that the knowledge would benefit the client.
The novel corona virus has changed all that. We can’t sit back in the safety and security of our therapists’ chairs, listening with compassion and objectivity to our clients’ struggles with isolation, fear of loss, separation from loved ones and the mundane facts of everyday life: where will I be able to buy toilet paper? Now I’ve got to do my own manicure for the first time! Oh no! We’re all in this together. Many therapy sessions – all virtual now, of course – begin with a client asking “So how are YOU doing?” Not the way we normally start a session! And there’s no way any of us would take that simple question and turn it around in the way we might have done in the past, by asking a question to the question, such as, “What makes you curious about that?’ No, these days, we’ve got to find a simple and ideally brief answer that says something authentic about how we’re doing. And then deftly shift the focus back to the client and what they need to discuss that particular day.
Starting out as a technology skeptic, I’ve been surprised to discover how much I’m enjoying Zoom therapy sessions. For one thing, I feel grateful to be able to continue working and seeing my clients in this highly stressful time. Even when I’m exhausted (and everyone agrees virtual sessions are more exhausting than in-person!) the gratitude never entirely leaves my awareness. At the same time, I’m also aware that many of the manifestations of anxiety and depression that we typically address in therapy are plaguing us on the other side of the couch. Anticipatory anxiety: what if this happens? What if that happens? I often guide clients back to the present moment to help them quell such future-oriented anxious thoughts. But I can’t do that so successfully now; none of us can.
Catastrophizing is another common anxiety symptom, one that I’ve prided myself on rarely falling victim to. But in these quarantine days, I too find myself imagining a scary future, worst case scenarios, our lives becoming unrecognizable in a kind of apocalyptic landscape. What? My inner therapist (who’s often asleep on the job these days) tells me to snap out of it, be realistic – not pessimistic! Then I look out one of the windows in my apartment and see so many people now wearing face masks and the street scene does in fact look like something from a sci-fi movie.
Poor attention span also seems to be a common side-effect of spending countless days cut off from the normal activities of our lives. I find myself starting to read an article in the newspaper (yes, I still read an actual paper newspaper) or a book review and within minutes, my mind is wandering and I’m turning the page to something else, leaving the thing that had caught my eye unfinished. I return to it again later and sometimes I’m able to plow through, sometimes actually recapturing the enjoyment of reading I’ve experienced since childhood. Luckily, doing the work we do isn’t challenging in this way: having the active participation of another person, albeit on a screen, keeps me engaged; I don’t have to rely solely on internal motivation – my clients keep me involved and motivated.
Many people are talking about mood swings, not necessarily the most dramatic kind, but being aware that one day or part of a day they’re feeling “okay,” able to get work done, able to feel reasonably confident in their ability to cope and then the next day, or later that night, their mood darkens, they feel lethargic and less able to imagine an optimistic outcome or even being able to manage the uncertain future we have in front of us. When I’m zooming from one therapy session to another, feeling inspired by the willingness and intentionality of my clients to keep the work going, to talk about family dynamics, relationship challenges, issues with self-esteem, the bedrock of psychotherapy, my mood is on the upswing. In the silence of an evening, after all the work is done, I may find my mood drifting downward. Time to peruse social media; time for Netflix – ideally something on Comedy Central (John Mulaney is a new favorite of mine) or to find an engrossing documentary like “Tiger King;” time to talk with my adult children or a close friend, not knowing when we’ll see each other in person again.
Legislation & Advocacy | Federal
Laura Groshong, LICSW, Director, Policy and Practice
What Will “Normal” Psychotherapy Become?
With videoconferencing and (thankfully!) audio psychotherapy, the possibility that we will no longer be forced to maintain the distancing that led to these forms of practice is beginning to emerge. What we can expect in the near to later future is at best likely to vary from state to state and region to region. Even the savviest crystal ball is looking cloudy!
Telemental Health Changes and Challenges
I have heard from clinical social workers from all over the country: the vast majority have moved in the past two months to doing psychotherapy through videoconferencing and telephonic means. I think it is safe to say that, while LICSWs used to feel frustrated by low reimbursement rates, lack of coverage for more than once a week treatment, and treatment reviews for psychotherapy that lasted more than a year, we now have a whole new set of frustrations.
A major challenge right now is the widespread discrepancy in terms of which private insurers and ERISA plans will cover videoconferencing and audio psychotherapy, which insurers and ERISA plans will cover or waive co-pays, and which insurers and ERISA plans will pay for videoconferencing/audio therapy at the same rate as in-person therapy. Of course the anxiety we face about becoming infected or infecting others colors everything we do, effectively rendering our insurance concerns less meaningful. And somehow, despite change and challenge, chaos and frustration, we persevere and try to maintain our professional and personal lives.
What will our practices look like in another 8 weeks, in 6 months, in a year, or maybe three years from now? We have no idea. Different states are following very different trajectories based on the way COVID-19 is impacting the people who live there. Indeed, some states are coping both with “Hot Spots” and, at the same time, with areas which are not only unscathed but demanding a return to “normal”.
So far, our state and local governments have been trying to create guidelines that will protect as many people as possible, mainly through physical distancing, hand washing, wiping down all high touch surfaces, and masks. That is the legal “frame”; we all still have to determine what we think is safe in doing our work in the present and moving forward.
Future of Telemental Health
Moving forward, is there a future for telemental health? Most important, according to my admittedly cloudy crystal ball, will be whether Medicare decides to maintain the expanded videoconferencing and audio psychotherapy, once the current restrictions in physical distancing are removed. Medicare policy generally impacts all the private insurers. Current physical distancing restrictions will be cut back on a state by state basis, so it is hard to say when CMS will decide there is “enough safety” to insist that all Medicare beneficiaries be treated in-person. Or indeed, will Medicare make such a decision? Will they have collected data and assessed the impact of videoconferencing and audio psychotherapy to determine whether these formats are as helpful as in-person face to face treatment? Are these formats effective tools for short term relief of mental health problems? For long term changes sought? How do they compare for in-depth trauma related treatment? It seems likely, too, that there will be questions of how much more or less expensive it would be to allow these forms of treatment to continue, where appropriate and effective.
CSWA will continue to work with CMS, HHS, and other national organizations to preserve the options that we now have, insofar as they are appropriate and effective, even after the crisis has abated. As you know, the predictions of when that will occur range from 3 months to 3 years.
Dealing with Insurance Issues in the Here and Now
Meanwhile, what do we do when insurers state they will cover the co-pays, pay the same amount for distance therapy as in-person therapy, describe which POS code and modifier to use, and then fail to reimburse according to these stated policies? These problems are some of the most frustrating we face. Spending hours tracking down provider liaisons about why our claim was denied, or paid at a lower rate, is painful and even scary. One remedy is to engage our patients in the process of finding out what their current co-pay coverage is. Keep a list of POS and modifier guidance as it comes out, by insurer, and keep it updated. If you find inconsistencies, let your insurance commissioner and attorney general know. This is the best way to get action on insurers’ failure to pay us what they have agreed to when we have complied with stated policies.
In other words, use your own judgment about what practice system feels safe for you and your patients and let insurers know that they need to be consistent. And most of all - stay tuned.
Laura Groshong is the Director, Policy and Practice for the Clinical Social Work Association.
In This Issue | JUNE 2020
Membership Dues Tax Deductible Amount: For the 2019 tax year, the percentage that is not deductible for tax purposes will be 24%, based on our projected lobbying expenses. 76% of your membership dues is deductible as a valid expense.
Legislation & Advocacy | District of Columbia
Adele Natter
Many people have expressed interest in how the DC Board of Social Work would change license requirements during the current pandemic. The Board met remotely on Monday, April 27, and discussed changes to its policies. The temporarily-revised policies are now posted on the website of the DC Board, in the Policy Guides and Statements section. Licensees are encouraged to check the website now for important details which may affect your practice. Keep an eye out for additional updates, particularly as DC’s State of Emergency regulations change.
Telehealth policy:
Social workers can practice using audio, visual, and telephone, as long as they practice within ethical and HIPAA standards of care. This policy will be in place until 12/31/2020, at which time it will be reconsidered.
Licensure Waivers during Covid-19:
Practitioners who are licensed in good standing in other jurisdictions may continue to serve clients who are in the District during Emergency conditions.
LGSWs in Private Practice:
LGSWs working toward advanced licensure may not practice independently, but can practice in another’s agency or private practice. An LGSW must be supervised by an LICSW.
CE Requirements for current License Renewal period:
For the current licensure period (ending July 31, 2021), the Board will accept online training, including pre-recorded offerings. Specific requirements for CE hours of ethics, LGBTQ, and public health issue trainings remain, but none need to be face-to-face.
The next meeting of the DC Board will be June 22nd.
Adele Natter, LICSW, Co-Chairs the GWSCSW Legislation & Advocacy Committee for DC with Margot Aronson, LICSW. Adele has been an active participant on the Committee for the past four years; she represented GWSCSW on a Board of Social Work sub-committee, which included NASW and CSWA representatives. Adele maintains a private practice focused on helping individuals with anger and emotional regulation issues. She is also a Clinical Instructor in the Psychiatry Residency Program of the George Washington University Medical School. She holds a BA in Psychology from UCLA and received her MSW from the University of Maryland.
Legislation & Advocacy | Maryland
Judy Gallant
This report is based, in part, on the multi-page summary of this year’s legislative session from our lobbyist, Pam Metz Kasemeyer, JD. Additional information about the 2020 session will appear in the September newsletter.
To state the obvious, the impact of the global pandemic has been profound, for each of us individually, for our clients, for our country, and for the State of Maryland. The changes that Executive Orders, given by the President and by our Governor, that have had a tremendous impact on our practices are covered in the Toolkit for Virtual Practice, above in this newsletter.
Changes to fight the pandemic
The shape of lawmaking during the yearly session of the Maryland General Assembly changed dramatically this year, as the session ended 3 weeks earlier than scheduled. The Covid-19 pandemic necessitated quick changes to the Maryland budget for Fiscal Year 2021. The State has spent nearly $2 billion responding to the Corona virus so far.
Some other actions taken during the shortened session:
Senate Bill 245/House Bill 527: Health Occupations – Social Workers – Scope of Practice, Supervision, and Application Decision Appeal Process (passed) was introduced to clarify language in a bill passed in a previous year that governs our practice. It was enacted with amendments requested by MdCSWC. The bill clarifies that “practice social work” includes counseling for alcohol and drug use and addictive behavior. For an individual licensed as an LGSW or LCSW, the bill further clarifies that “practice social work” includes treatment of biopsychosocial conditions under the supervision of an LCSW-C, an amendment offered by MdCSWC.
ACA and Parity issues
Concern over the fate of the federal Affordable Care Act (ACA) prompted legislators to pass House Bill 959/Senate Bill 872: Health Insurance – Consumer Protections (passed). The bill is an emergency bill which codifies the patient protections contained in the ACA rather than simply referencing them in a cross-reference to the federal statute. During the 2019 Session, the Maryland Health Insurance Coverage Protection Commission was required to establish a workgroup to (1) monitor the appeal of the decision regarding the ACA and the implications of the decision for the State; (2) monitor federal enforcement of the ACA; and (3) determine the most effective manner of ensuring that Maryland consumers can obtain and retain quality health insurance. This bill generally implements the recommendations of the workgroup.
Continued concern over network adequacy issues in behavioral health prompted House Bill 455/Senate Bill 334: Health Insurance – Mental Health Benefits and Substance Use Disorder Benefits – Reports on Nonquantitive Treatment Limitations and Data (passed). This bill requires carriers to submit two reports (in 2022 and 2024) to the Insurance Commissioner to demonstrate compliance with the federal Mental Health Parity and Addiction Equity Act and provide information on benefits. With regard to the latter, this report is limited to the frequency, reported by number and rate, with which the health benefit plan received, approved, and denied prior authorization requests and the number of claims submitted for mental health benefits, substance use disorder benefits, and medical and surgical benefits in each Parity Act classification during the immediately preceding calendar year.
Education issues
You may remember that last year I wrote about efforts to pass legislation to create guidelines on a trauma informed approach in Maryland schools. Although the efforts failed last year, this year those efforts to develop guidelines for schools on a trauma-informed approach succeeded with the passage of House Bill 277/Senate Bill 367: State Department of Education – Guidelines on Trauma-Informed Approach. The Maryland State Department of Education (MSDE) must create guidelines in consultation with MDH and the Department of Human Services, and MSDE must distribute the guidelines to local school systems and publish the guidelines on its website. A “trauma-informed approach” is defined as a method for understanding and responding to an individual with symptoms of chronic interpersonal trauma or traumatic stress. A “trauma-informed school” is a school that: acknowledges the widespread impact of trauma and understands the potential paths for recovery; recognizes the signs and symptoms of trauma in students, teachers, and staff; integrates information about trauma into policies, procedures, and practices; and actively resists re-traumatizing a student, teacher, or staff member who has experienced trauma.
As you may remember from the article by Katie Smeltz in our last issue of News and Views, the Kirwan Commission on Innovation and Excellence in Education was charged with setting new education funding formulas and developing recommendations to transform the state’s public education system. After more than two years of deliberation, the Commission’s recommendations were reflected in House Bill 1300: Blueprint for Maryland’s Future – Implementation (passed), which was enacted by the General Assembly and awaits signature by the Governor. The legislation includes a comprehensive set of strategies for enhancing school-based behavioral health services, which have been shown to improve student health and education outcomes.
The bill dedicates staff at the Maryland State Department of Education (MSDE) to coordinate with school behavioral health services coordinators, requires training of school personnel in protocols to support students in need of behavioral health services, and requires each local school system to develop and implement systematic screening to identify students with behavioral health needs.
The $4 billion bill plans many additional changes, including establishing a Consortium to develop and fund community-partnered school behavioral health programs across the state, provide free pre-kindergarten statewide, boost teacher pay and standards, and give extra money to schools with large populations of economically disadvantaged students. However, the State’s response to the Coronavirus and the anticipated decrease in revenue is putting the funding for the plan in jeopardy. Although the bill passed both the Senate and the House with a veto-proof majority, it is unfortunately not clear that the funding will be available to move forward with the plan in the coming year.
Ruling: Physical incapacity includes cognitive deficits
Early in May, the MD Court of Appeals (our highest court) unanimously held that the phrase "physical incapacity" includes cognitive deficits. The ruling was narrow but the precedent is broad. Interpreted maximally, the Court said that mental illness, PTSD, & brain injury are "now known to be manifestations of a physical incapacity."
Released quietly during a pandemic, this ruling is a major win for those who fight for mental health parity, for service-disabled veterans, and victims of brain injury. (This information is courtesy of MD State Senator Jeff Waldstreicher.)
Judy Gallant, LCSW-C, is the director of the Society’s Legislation & Advocacy program, as well as chair of the Maryland Clinical Social Work Coalition, our GWSCSW legislative committee in Maryland. She maintains a private practice in Silver Spring.
Pamela Metz Kasemeyer, JD, and her firm of Schwartz, Metz & Wise, PA, represent us in Annapolis and guide our advocacy strategy. Ms. Kasemeyer is an acknowledged authority on Maryland’s health care and environmental laws and has represented a variety of interests before the Maryland General Assembly and regulatory agencies for more than 25 years.
Legislation & Advocacy | Virginia
Judy Ratliff
Board of Social Work Changes to the Regulations Governing the Practice of Social Work
- There will be a reduction in fees for the initial licensure for Licensed Baccalaureate Social Workers( LBSW) from $115.00 to $100.00 and the annual renewal fee is reduced from $65 to $55.
- The most significant reduction in regulatory burden is the elimination of the current requirement for an applicant with a baccalaureate degree to have 3000 hours of supervised experience in order to qualify for licensure as an LBSW. THIS REPRESENTS A HUGE CHANGE. BSWs, PLEASE NOTE.
- The number of hours of continuing education pertaining to ethics or standards of practice effective as of 11/13/2019 is an increase from 2 to 6 hours for LCSWs and from 2 to 3 hours for LBSWs and LMSWs.
- Licenses will be renewed as usual in 2020, but the completion of 30 CEUs for 2020 and 2021 combined will be delayed until 2021. Thus, two years of CEUs will be due when licenses are renewed in 2021.
- The Board will cease to mail hard copies of licenses, certifications and registrations. The Board will issue a final hard copy that has no expiration date. The renewal period will begin in May and the Board will send out email notices at that time. You will have to maintain the final copy. Insurance providers, employers, boards and citizens may obtain this information on "License Lookup". Replacement or duplicate of a hard copy license, certification or registration may be requested through an individual online account NOTE: The content on License Lookup meets the accreditation standards for primary source verification from the top seven accreditation organizations for healthcare professionals. This could be a source for those of you looking into getting accredited in other jurisdictions.
- Two separate licenses, LBSW and LMSW (masters) are now in effect.
Laws Passed by the Virginia Legislature and Signed into Law in 2020
- The Governor approved SB 1046, Clinical social workers; patient records, involuntary detention orders, effective 7/1/2020. The bill adds clinical social workers to the list of eligible providers that includes treating physicians and clinical psychologists, who can disclose or recommend the withholding of patient records, face a malpractice review panel and provide recommendations on involuntary temporary detention orders.
- Proposed Study: There was a recommendation that the Department of Health Professions convene a work group to identify the number of social workers needed in the Commonwealth to adequately serve the population; identify opportunities for the Commonwealth's social work workforce to successfully serve and respond to the increasing needs of individuals, groups and communities in a variety of areas such as child welfare, aging, mental health and other areas of social need; gather information about current social workers in the Commonwealth related to level of education, gender, employer and compensation; analyze the impact of compensation levels on social workers' job satisfaction and performance and other aspects; and make recommendations for additional sources of funding to adequately compensate social workers and increase the number of social workers in the Commonwealth.
- HB 42: Prenatal and postnatal depression, etc.; importance of screening patients: Under this bill, doctors who provide primary, maternity, obstetrical or gynecological health care services pertaining to prenatal or postnatal depression or other depressions are to provide screening for these diagnoses for every patient who's is currently pregnant or who has been pregnant within the previous five years.
- The numerous laws previously put in place limiting a woman's access to abortion were repealed, including the mandatory 24 hour waiting period and ultrasound testing.
- Dozens of Jim Crow era laws that limited the rights of black Virginians were removed from the code as these laws had been declared unconstitutional by federal courts years ago.
- The Virginia Values Act prohibiting discrimination in housing and employment for all persons passed, making Virginia the first state in the South to do so.
- A bill was passed that added protections of the hate crime law to all persons regardless of sexual orientation or gender identity, as were other bills to prohibit LGBTQ discrimination. Conversion therapy for minors is banned under a new law.
- Major bills passed to make voting easier. No-excuse absentee voting was enacted, and election day will now be a holiday. A repeal of the photo ID requirement for voting passed.
(Please note that summaries of the bills in items 4-8 are courtesy of Delegate Ken Plum, Reston)
Judy Ratliff, LCSW, (recently retired from work but not from GWSCSW or from life) Co-Chair, VA Legislation and Advocacy Committee.
Announcing a New Co-Chair for the Northern Virginia branch of the Legislative and Advocacy Committee
I am thrilled (and I'm not kidding) to announce that I now have a super-qualified co-chair in the person of Wayne Martin. Wayne was the first president of the VSCSW when it was formed in 1991. He served as president from 1991-1995. He was appointed to the Virginia Board of Social Work by Governor Mark Warner in July, 2004 and was reappointed by Governor Tim Kaine in 2008. He became Chair of the Board in July, 2010 and served out his term until June, 2012. Wayne was awarded the Lifetime Achievement award by the Virginia Society for Clinical Social Work in 2019.
Wayne was in private practice for over 30 years and worked for the Navy as a civilian until his retirement in December, 2019. He moved from Norfolk, VA to Bethesda, MD in early January of this year and joined the Greater Washington Society of Clinical Social Work. I am looking forward to having his expertise and sharing this position with him. Welcome, Wayne.
AThe Stages of Grief in Quarantine
By Gina Sangster, MFA, MSW, LICSW | Psychotherapist & Supervisor, Capitol Hill Consortium for Counseling & Consultation
 I
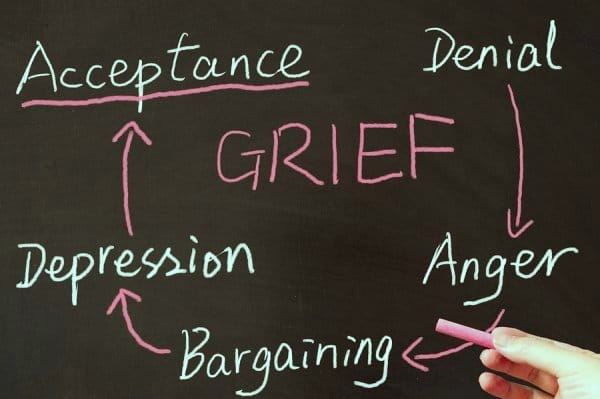
definitely hit the Anger stage of grief in the middle of week-4 of our
stay-at-home order. As anyone knows who has experienced grief and loss, the
stages are not sequential. We used to like to think you could progress in a
neat pattern from one to the other, finally culminating in a sigh of “Acceptance.”
Actually, I’ve heard it suggested that Acceptance may be too tall of an order
and that the best we can hope for is Understanding. We may never get to full Acceptance in many grief and loss scenarios. Will we ever fully accept the way
the Corona virus has upended our world? But let’s get back to the Anger stage, as
I’m nowhere near Acceptance OR Understanding.
I
definitely hit the Anger stage of grief in the middle of week-4 of our
stay-at-home order. As anyone knows who has experienced grief and loss, the
stages are not sequential. We used to like to think you could progress in a
neat pattern from one to the other, finally culminating in a sigh of “Acceptance.”
Actually, I’ve heard it suggested that Acceptance may be too tall of an order
and that the best we can hope for is Understanding. We may never get to full Acceptance in many grief and loss scenarios. Will we ever fully accept the way
the Corona virus has upended our world? But let’s get back to the Anger stage, as
I’m nowhere near Acceptance OR Understanding.
Today, I hate my toaster oven. Let’s be clear: I love my toaster oven. I’m not sure how I could survive without a toaster oven. Anyone who knows me knows I love things crispy and toasted. Don’t give me a pale, lukewarm English muffin; it has to be golden – darker around the edges. Even a little burnt is okay. And I’ve got a stockpile of bread supplies to choose from in my refrigerator: Trader Joe’s cinnamon roll bread, the above-mentioned English muffins, seedless rye and pita. I’m well-stocked for this quarantine. Yes, there’s spinach and broccoli too, but this is not the time I’m going to curtail my carb addiction. Actually, no time is that time for me; but especially not now. The thing is my toaster oven is very loud when it announces your toast is done. And today, this causes me to feel furious as I lift out the lovely slices onto a waiting plate. This is not a normal reaction, but it’s normal under these circumstances.
I’m having fantasies of escape, which fits right in with the Bargaining and Denial stages. This morning I was plotting how I’d put on a mask and gloves and go to the post office and CVS. I wouldn’t confess this to my adult daughters or son. Earlier this week, in a half-awake, half-dream state, I imagined pancakes and scrapple from Eastern Market Lunch (I know, I know, one of the worst foods in the entire world; but my mother used to fry scrapple, so you can understand my longing). I could just sneak over there and no one would know, right? Once fully awake, I recognized my fantasies as hallmarks of Bargaining and Denial; the hopeless wish to dupe reality, to find a way out of a reality that seems unbearable.
I believe in every family, every friend group, work group and neighborhood, there are the Corona virus gatekeepers. These are the people who were early adopters of quarantine. In my family, it’s my eldest daughter. She hasn’t left her house since early March and no one is allowed in or out except her immediate family – my son-in-law and two grandsons. She recently allowed her sister, who lives twenty minutes away, to visit on the deck, touching no one and not being allowed into the house for any reason. She has a history of asthma and one of my grandsons has asthma, so this all makes sense; except there are moments when it feels dictatorial and irrational. If I even allude to doing something, or refer to something someone else has done that skirts the edges of safety, her reaction is swift and unyielding. She’s that parental figure, telling you your strict curfew is for your own good, and there’s no room for negotiation.
Some of my Anger and Bargaining, springs from how highly I value self-sufficiency. There have been moments when I feel like (and in my own head, sound like) my early twenties client who has a tendency to whine. Trust me: she won’t mind if she reads this: we have an open dialogue about where the whining comes from and why it’s so difficult to openly express feelings, needs and opinions. I think she’ll actually appreciate knowing that I whine too. I hear myself whining about not being able to do all the things I normally do, go the places I want to go (granted, most of them are closed now). Yes, people are helpful and more than willing to bring me groceries, but I want to go get them myself, as I’ve always done! During the first week of the shut-down, this young woman was the voice of the resistor, the person who didn’t want to believe any of it and didn’t want to adjust her behavior. Of course, she has since come around to living life sequestered at home, like the rest of us. But sometimes, we still want to protest, to deny the unbelievable, surreal world we now inhabit.
I’m sure we’re all familiar by now with the Depression that comes with isolation. The lack of motivation; worries about the future, poor self- image because we’re not exercising, being productive, or receiving stimulation from any of the external resources we’ve come to rely on. The work we do as therapists is in one way easier than other kinds of work that can be done virtually because we receive the engagement of our clients; we don’t have to be entirely self-motivated. But it’s still hard, for all of us, especially those who have lost jobs, whose incomes are now slashed, those who toil on the front lines in hospitals, those who still stock our supermarkets and pharmacies.
Recognizing the stages of grief can help: Denial, Anger, Bargaining, Depression, Acceptance – or Understanding, and recognizing that the stages don’t progress in any neat order. We will all cycle through repeatedly, finding ourselves suddenly angry at an inanimate object – or worse, a loved one; suddenly gripped with sadness because we haven’t seen our friends, the inside of a gym or yoga studio or anyone else for that matter, except on Zoom. It has recently been suggested that we add a sixth stage of grief: Meaning-making. I’m sure the process of trying to make meaning of this pandemic will consume many hours and in many great minds. Meanwhile, let’s be kind to one another and to ourselves, and to all the people (and even objects!) that are helping us get through this.
By Gina Sangster, MFA, MSW, LICSW | Psychotherapist & Supervisor, Capitol Hill Consortium for Counseling & Consultation
 At the closing of a virtual gathering, a member of a grief and loss group that I facilitate said that she wanted to “give herself grace” at this time of isolation. Her words stayed with me.
At the closing of a virtual gathering, a member of a grief and loss group that I facilitate said that she wanted to “give herself grace” at this time of isolation. Her words stayed with me.
During my first week of self-quarantine, I purchased an on-line yoga practice and logged onto one of the first Zoom classes my local yoga studio offered. I’m also supposed to be continuing with daily rehab exercises for the knee replacement surgery I had in December. Though going to physical therapy was hard and time-consuming, DIY is much harder. I’ve partnered with a neighbor who had the same surgery in January so we can at least support one another by phone. I get daily reminders from the on-line yoga practice and I know the local studio is continuing to offer virtual classes, but I haven’t participated since that first week. I’m probably doing about a quarter of the exercises my physical therapist sent me by email; the stiffness in my knee in the middle of the night and when I wake up every morning tells the tale. She also advised me to take daily 20-30 minute walks; that was before the pandemic death toll reached record numbers, before our Mayor directed us to “Stay At Home.” Now we’re advised to wear masks. Should I venture out? At what risk? I’m trying to give myself grace.
Like many people who didn’t come of age with cell phones, smart phones, tablets and laptops, I often try to limit reliance on my I-phone. Plug it in to recharge some distance away. Turn off the ringer. Don’t check email; don’t reply right away to texts. All of this has gone out the window in isolation. I carry my phone around my apartment like a baby bird held delicately in my hand, fearing for its life. But it’s really the phone that is my lifeline, kept close by at all times, not always on but always accessible. And even when I’m brave enough to silence it, I frequently glance at its blackened screen to see if any messages have appeared. Sitting down to write or read, I may silence it and turn it over so I can’t immediately see the screen; but any minute now I’ll feel compelled to check. Are we all developing aspects of obsessive compulsive disorder? I’m trying to give myself grace about that too.
A few years ago, I finally gave up my land-line. Confession: I hadn’t actually had a telephone attached to the line for a few years prior, but I had a hard time giving up the number, a vintage 1970’s era impossible-to-forget set of digits. I kept paying the basic fee, planning to get a new phone or cut off the service altogether. Now I wish I had that old-school backup. Like many of the clients I see for psychotherapy, I’m struggling with anticipatory anxiety: what if something happens to my cell phone? You can’t just go down the street as usual to the AT&T store. Sure, you can order from Amazon, the demigod of life in the twenty-first century, but would I get what I want? How much would it cost? How long would it take to arrive? What would I do in the meantime? Not being able to reach my adult children in New York or Portland, Oregon? Lose contact with clients, colleagues, friends? This is the kind of negative ruminating I’ve never fallen prey to before in my life and that I hear all the time from people who come to me for therapy. Up until now, it’s been easy for me to spot this predilection, to hear the repetitive trains of thought that drive an ever-increasing track of fear and negativity and to offer observations and insight that can help derail such ruminations. A client recently told me she hadn’t realized she was allowing herself to imagine worst case scenarios so far into an unknown future until I pointed it out. That wasn’t long ago, before any of us imagined where we’d all be today. I felt gratified that I was able, with a few simple word, to help her realize something essential about her tendency to catastrophize, and to help her gain some control that can come with self-awareness. Right now, I’m trying to give us all grace.
My 24 year-old son, living with his girlfriend in Portland, Oregon, told me he plans to learn German and improve his Spanish while practicing social distancing. An inveterate introvert, the transition to working virtually and spending quiet hours in isolation hasn’t been such a stretch for him. Plus, he’s got the attention and support of a loving partner. I won’t be surprised if he comes out of this speaking a new language and perfecting the Spanish he started learning in middle school. But for the rest of us mere mortals, let’s give ourselves grace.
Poem in the Time of Covid
By Judy Ratliff
I walked down a corridor I didn't know.
It was the corridor of fear...
the fear of a freefall into the unknown.
And unknown and unknowing, I walked the corridor of fear.
And then i was joined by grief,
a cloak that covered me and
almost smothered me with sadness so severe that I almost forgot that this was the corridor of fear.
Fear, grief, change.
The swirling mists of change engulfed me
as I walked very near to the end of the corridor of fear,
very close to being fully gripped in grief.
Then the mists around the unknown change began to clear
and I could see that something new was near.
And the unknown expanse of change appeared,
beckoning to be explored.
Consider advertising in the next issue of News & Views
Post ads for:
- continuing education training,
- office space, upcoming groups,
- job opportunities, specialized services, etc.
Please get in touch with Donna Dietz, GWSCSW Administrator (admin@gwscsw.org) to reserve your space in the next issue.
Don't forget -- we offer free design for your display ad!

The Mentor Program is always looking for new mentors to work with newer social workers who are looking for guidance and help as they start their careers. You determine how much time you want to give; this is worked out with the mentee. For questions, please contact Nancy Harris, Coordinator of the Mentor Program, at (301) 385-3375, or nlharris1214@gmail.com. Thank you for your support of this important benefit of GWSCSW membership! |
Communications Branch
Kate Rossier, Director of Communications | Email: kazrossier@hotmail.com
As this is my last Communications Branch report, I would like to thank you all for the pleasure of serving in this capacity. My efforts have been to work with Donna Dietz, our administrator, to improve and strengthen our website and oversee the newsletter, listserv, and social media communications. I also give great thanks to Nancy Pines, who has done a splendid job with our newsletter these last two years and will be continuing on; Joel Kanter, who continues to be our listserv moderator and sends articles of interest out for all of us to read; and to Chana Lockerman, who is our ongoing social media chairperson and writer of the interesting articles on technology for the newsletter. You’ve all been terrific! - As I leave this position, I will be turning over these efforts to Steve Szopa, former president of the society. He will bring his own great energy to our communications and I’m sure will make improvements on all fronts!
Please send any questions, suggestions, feedback or comments to admin@gwscsw.org.
Education Branch
Susan Post, Director of Education | susan.post@gmail.com
What an unusual year. Coronavirus obviously had a negative impact on our ability to present continuing education programs for GWSCSW members. Even before the general shut down, the continuing care communities we use as venues for our workshops discontinued their availability to outside organizations and visitors. Numerous scheduled programs had to be either postponed to next fall/winter or conducted online. Yet this will mean a busy and rich schedule for the coming year when, with any luck, we will be able to reconvene.
We will have a new Director of Education, Leila Jelvani, who has worked with me on programing this past year and is eager to launch an exciting schedule. She will be assisted by Robin Seiler and Jackie Fonseca; many thanks to each of them for stepping up.
Sadly, the annual Alica Kassabian Memorial Conference, which typically takes place in November, has been cancelled. This lecture brings an outside expert to DC and involves travel, housing, venue and food reservations. It was felt by the conference committee that, given current uncertainties, it would be best to postpone. 2020 would be an “off” year for our semi-annual ethics conference with Frederic Reamer, so we will look forward to his return in 2021.
Despite the effect of Covid 19 on continuing education during the latter part of the year, we had lots of rich programming during fall and winter of 2019-2020. Many thanks to the presenters of these workshops. If you are interested in offering a workshop for our membership for the coming year, please feel free to contact Leila Jelvani at leila.jelvani@gmail.com.
Wishing everyone a safe, healthy, if unusual summer, and l look forward to reconnecting in the fall.
Leila Jelvani: leila.jelvani@gmail.com
Shauna Alonge: salongelaw@gmail.com
Robin Seiler: rsseilerjr55@gmail.com
Legislation Branch
Judy Gallant, Director of Legislation| Email: judy.gallant@verizon.net
This is a time unlike anything we have ever experienced. As I write this, most of us have been sitting in front of our computers to see clients, practicing completely virtually, for over 6 weeks. Our lives are spent primarily in our homes, save for the walks or runs we can grab outside, the stealthy trips to the grocery store, masks and gloves in place (that is, if we can’t manage to snag an Instacart slot), and yardwork. Who ever thought mowing the lawn and picking up windblown branches would be a respite? Yes, I know some people love gardening. I have not typically been one of them.
We struggle to get used to the situation, but how long will it last? When will we feel comfortable returning to our offices and seeing people in person? When will our clients be willing to come to our office, after they’ve been able to see us from the comfort of their homes? WHEN WILL OUR CHILDREN RETURN TO SCHOOL? When will we get to hug our friends – or our adult children and our grandchildren - again? And how do we cope with our own fears of getting ill and dying alone?
And the billing of those damnable insurance companies – will it ever make any sense? Why can’t they just standardize their coding and let us get our payments promptly? Do I use 95, GT, 02, GQ or maybe BS?? Perhaps answers lie amongst the thousands of emails from the past 2 months? Let’s see:…oh, here’s an answer! Yes?…No…here’s a different answer!
- Is this a new reality?
- Was this our old reality?
- Or is this a coronavirus nightmare?
I close my eyes, and as if dreaming, my mind’s eye brings into focus the image of a toolbox! There’s writing on it! It’s a hyperlink! It’s from our Society’s website, posting all of the information one will ever need in this time of telehell: https://www.gwscsw.org/covid-toolkit. Yes, it’s there!! Yay! Wow, look at all that information. OMG-it’s even been updated!! Thank goodness I’m not alone with this. This community is great!
Oh, and what’s this? There’s even a link to the CSWA website for a sample consent form for telemental health treatment. Do I have everything I’m supposed to have on my consent form, I wonder,…and did I join CSWA this year? I really meant to. OK, I’d better do it right NOW, since I just know I’ll forget. OK, that feels a bit better. And, it’s amazing, I actually got my billing done, the way I think I’m supposed to.
What’s this, a new piece of information? It looks like those stupid insurance companies changed the process from what the toolkit said! OK, good. I’ve finally gotten it right and now I’m getting paid.
Probably not too many people have seen what I just noticed. Hmmm, I should let Judy G know about that change so the website can be updated. It feels good to contribute that information to my colleagues and my friends. I want to do this more often, spend some time helping with advocacy. The Legislation and Advocacy group probably could use my help now more than ever.
Be sure to contact one of us with any questions, suggestions, or information you might have, or to join one of the committees: in DC, Margot Aronson at malevin@erols.com or Adele Natter at anatter@verizon.net; in Maryland, Judy Gallant, judy.gallant@verizon.net; and in Virginia, Judy Ratliff, jratliff48@hotmail.com. We look forward to hearing from you.
By Chana Lockerman
With gratitude to Tech Tips for many years of service, the Social Media Committee celebrates this column’s retirement. We’re excited to announce a new column that reaches beyond the “how-to” perspective of Tech Tips and explores the dynamic relationship between technology and social work, and how social workers interact with technology in our ever-changing world.
Years ago when Tech Tips was born, many GWSCSW members were first working out how to integrate technology into their social work practice. We’ve come a long way since this column first helped to manage email, electronic medical records, and what we now consider the basic technologies of the mental health field.
Our new column is here to serve you, so it’s only right that you name it! Please submit your suggestions to name our new column to chana@rockcreekcounseling.com.
Cecilia McKay, MSW, is graduating from the two-year Psychoanalytic Studies Program at the Washington Baltimore Center for Psychoanalysis and has been accepted as a third-year analytic candidate in the Institute. She has a private practice in Rockville, Maryland.
Committee Reports
Continuing Education Committee
Shauna Alonge| Leila Jelvani
cecommittee@gwscsw.org
Click here to submit a proposal. Once submitted, the proposal will be reviewed by the Education Chair and the Continuing Education Committee.
Legislation & Advocacy Committee
Judy Gallant
dirlegislation@gwscsw.org
Membership Committee
Cindy Crane, Nancy Harris, Catherine Lowry
membership@gwscsw.org
Mentoring Committee
Nancy Harris
mentoring@gwscsw.org
The GWSCSW Mentor Program continues to be available during this time of social distancing. Mentors are available to meet online. If you’re interested in having a mentor to help you transition from school to workforce, to get started in your career, to answer questions about licensing and online continuing education please fill out the Mentee questionnaire located on the GWSCSW website. If you have questions about the GWSCSW Mentor Program, please contact the coordinator, Nancy Harris, LCSW-C, at (301) 385-3375 or nlharris1214@gmail.com.
Newsletter Committee
Nancy Pines
npines12@aol.com
Your newsletter welcomes ideas and articles about clinical social work and practice. We are also very interested in hearing from members who have specialized knowledge or adjunct therapy practices they want to share.
Please consider your own life experiences and how they may have affected how you practice. One of the things I love about our profession is how we are always learning. Why not share your expertise and life lessons with fellow members? Send an email with your story/essays to npines12@aol.com. I'd like to give a shout-out to Gina Sangster, who contributed timely and relevant essays to this issue.
We now have three "proofers" (which AOL is always telling me is not a word, but whatever): Adele Natter, Shoba Nayar (both of whom have been doing this for several years), and Steve Szopa, our former president. Thank you for your willingness to check out my work!
Social Media Committee
Chana Lockerman
socialmedia@gwscsw.org
The Committee is excited to announce a new column that explores the dynamic relationships between social workers and technology. Please help us name the new column! Email Chana Lockerman: chana@rockcreekcounseling.com with suggestions about what to call the new column and what you’d like it to cover.
Volunteer Committee
Beth Pascoe
volunteer@gwscsw.org
GWSCSW Job BoardGWSCSW is proud to feature a job resource to connect career opportunities with our members. Visit the GWSCSW job board to look for jobs or to post a job today. Manage Your Career:
Recruit for Open Positions:
|
 Classified Advertising
Classified Advertising
Advertisements, accompanied by full payment, must be received by GWSCSW by the first of the month preceding publication. Material should be sent to admin@gwscsw.org. For questions about advertising, call 202-537-0007.
Adolescent/Young Adult Therapy: CBT, DBT, Medical Illness Counseling, Unified Protocol, Group Therapy. Powerful interventions for depression, anxiety, anger, perfectionism, fear, shame, rumination, social anxiety, ASD and more. Rathbone & Associates. Rely on Experts. 301-229-9490 www.rathbone.info.
Professional CEUs: Rathbone & Associates Professional Training Program. See our current schedule at www.rathbone.info, click on “Professional Trainings”. Current topics, quality speakers, practical skills.
Psychiatrist centrally located in Howard County seeking collaboration with licensed therapist in private practice setting. I am accessible, friendly and creative. I return phone calls, work with adult individuals and incorporate family/other support network into treatment and engage in diagnostic/treatment formulations with therapists. I provide in-office or telehealth appointments for MD, DC and VA. Based on the size of your practice, potential to provide on-site services. Fee for service only. Please see www.beginnersmindpsychiatry.com or contact me directly pjnegro@me.com 410 262-5621
Newly renovated, beautifully designed therapeutic space is available in Downtown DC, centered on Farragut Square, a 1-minute walk from both the Farragut North Red Line and the Farragut West Blue/Orange/Silver Lines. The secure building (with lobby attendant) is a rare find in DC, one of the few renovated downtown historic structures that also maintains original charm as a quiet, solid and beautiful space between modern high-rises. With natural light, wood floors, and intentional designs that facilitate and support a healing, prosperous, and professional space, the private suite consists of a waiting room, with the option to rent one or both of two additional private offices, available full or part time. Suite is fully furnished with flexibility for modifications and personal touches to suit individual taste and modality. To discuss further please contact: Emily Cooper, MPH, MOM, LAc @ 202.320.4213 or emilycooper@healingwisdommedicine.com
Located in Downtown Bethesda 2 blocks to metro and on the J2 bus line. Large, furnished, friendly office with ample natural light in very quiet therapists' suite, (two offices in suite). Large office consists of a desk area behind the sofa that faces two comfortable chairs area, storage space, locked closet with file cabinets and fax machine/copier. Large parking lot on site provides free parking for yourself and your clients. Suite also contains sitting area, water cooler, private bathroom, kitchenette and wifi. Building is open 24/7 with utilities on. Building is accessible currently during the Covid Crisis. You can use the office to see clients/patients remotely if you need a quiet space. Almost full time (minus 6 hours) for $995, or two days plus flexibility for $550 or make an offer. Contact Mona Mendelson | mona.mendelson@verizon.net | 240-354-6704 or Jolie Golomb | jbg5129@gmail.com | 202-390-4471
Ellicott City/Columbia, MD Office Space | Beautiful reasonably priced office space for rent part time with potential for full time, in Ellicott City/Columbia, MD. Fully and very nicely furnished, in suite with other cordial and collaborative therapists, lots of referral potential. Three-windowed corner office, with commonly shared kitchen, waiting room, free parking, swanky elevator building. Email njkillen@aol.com
Classified Ads: 75¢ per word | Minimum price $15 (20 words)
Display Ads: Full page 7 x 9¼ $325 | Half page $250| Quarter page $125 | Eighth page $75
Electronic submission (JPG) preferred. Publication does not in any way constitute endorsement or approval by GWSCSW, which reserves the right to reject advertisements for any reason at any time.
News & Views
Nancy Pines, Editor
News & Views is published four times a year: March, June, September and December.
Articles expressing the personal views of members on issues affecting the social work profession are welcome and will be reviewed and published at the discretion of the editor. Signed articles reflect the views of the authors; Society endorsement is not intended. Articles are subject to editing for space and clarity.
News & Views Submission Guidelines
Articles – Focus on your area of expertise and practice, ethical dilemmas, responses to events in the media or other topics relevant to clinical social work. Articles should be 500–700 words.
Out & About – Share news about you: an article you’ve written, if you’ve been in the news, taught a class, earned a new certification or are a singer, artist or writer. Submissions should be 50 words or less. Send all submissions to npines12@aol.com
Advertising: admin@gwscsw.org
Next submission deadline: August 30,2020
Need to reach a Board member? Click here for the listing of the GWSCSW Board of Directors

